Gene therapy has been developed in mice to treat sickle cell disease and β-thalassaemia. Further experiments on human cells suggest the therapy should work in people too, and a new test will determine how well patients respond to the treatment.
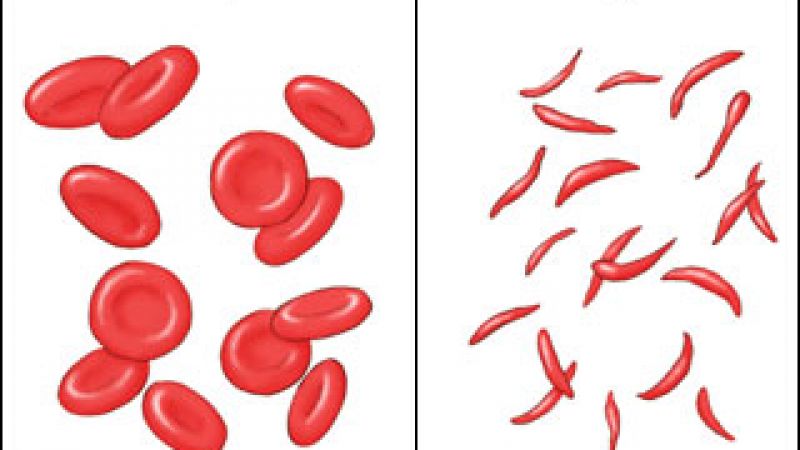
Sickle cell disease and β-thalassaemia are caused by different mutations in the haemoglobin gene resulting in faulty haemoglobin protein, low levels of the protein or none being produced at all. Haemoglobin is required to transport oxygen in red blood cells. The only cure for either disease is bone marrow transplantation, which can be rejected by the recipient’s body. Treatment of acute episodes is by blood transfusion.
So far, gene therapies for sickle cell and β-thalassaemia can replace the mutated genes with healthy copies, but they are relatively ineffective as they achieve only low levels of healthy haemoglobin production. The new therapy uses a specially developed gene, called an ankyrin insulator, which controls the structure of the DNA surrounding the gene, helping produce higher levels of healthy haemoglobin.
The therapy was administered by taking bone marrow cells from mice affected by either sickle cell or β-thalassaemia, treating them with the gene delivery system and then returning them to the mouse’s marrow. This markedly increased levels of haemoglobin and red cell counts in both diseases. Further studies showed the effect to be long lasting.
Tests using blood cells donated by patients indicate that the therapy works the same way in people as it does in mice. The team then developed a test that allows them to predict how successful the gene delivery system will be in patients depending on the genetic profile of the patient. This will improve the use of the technique in future clinical trials.
Last edited: 14 March 2022 09:00