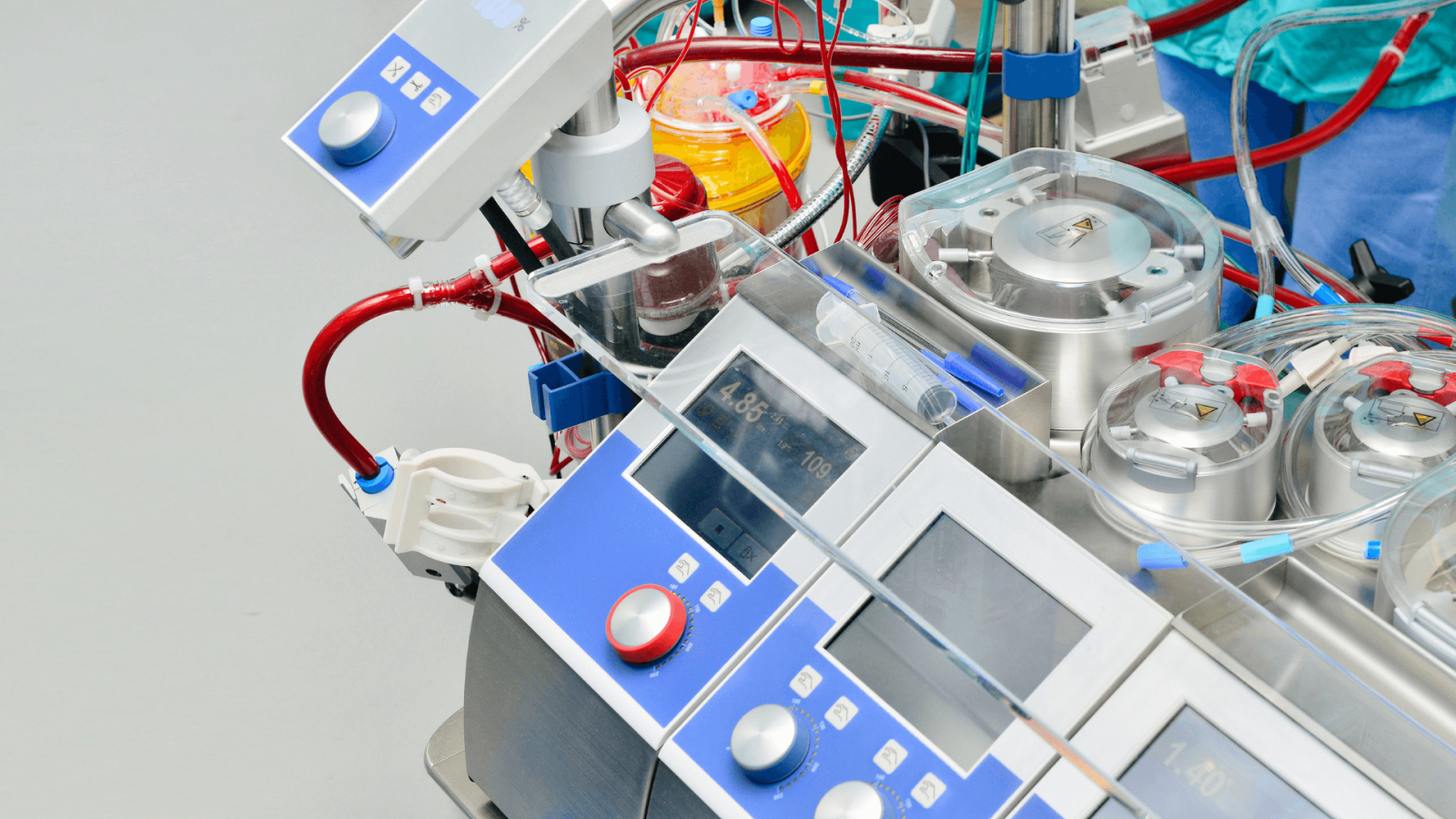
The cardiopulmonary bypass pump, or ‘heart-lung machine’ as it is commonly known, can take on the role of the heart and lungs during cardiac surgery. Operating on a beating heart is extremely difficult, and the heart-lung machine allows blood to bypass the heart while surgeons work. The machine is attached to the veins that feed the heart and to the arteries that leave it. It draws blood from a patient just before it reaches the heart, adds oxygen to it, and pumps it back around the body, ensuring that all of the organs receive the oxygen they need.
Like many medical advances, the development of the heart-lung machine depended heavily on animal research. In 1931, John Gibbon had been moved by the death of a patient during cardiac surgery. Convinced the patient would have survived if their blood circulation had been artificially maintained, he began to investigate the possibility of building an external device that could do the job of the heart and lungs for short intervals.
Gibbon and his wife carried out their initial research using cats, and by 1935 they had developed a machine that could replace the function of a cat’s heart and lungs for 20 minutes. These early animal experiments allowed Gibbon to test different types of pumps and oxygenators to improve performance, however, the machine damaged blood cells, and most cats lived no longer than 23 days after surgery.
From 1945, Gibbon and other researchers began to refine the method using experiments in dogs. Although initial survival rates were low, these experiments revealed the need to add filters to the heart-lung device to prevent blood clots, and to apply suction to the heart to prevent air from entering it during surgery. Once these issues were addressed, most dogs survived their open heart surgery, and the heart-lung machine was ready for use in humans.
In 1953 John Gibbon realised his 20-year vision and performed the first successful operation on a human using the heart-lung machine. The patient, Cecelia Bavolek, whose heart was connected to the machine for 45 minutes, recovered fully from the operation. However, the technique still had a major flaw; the heart was left beating during surgery with some blood still reaching it, and this made it messy and difficult to operate on.
The problem was again investigated using animals. Experiments in dogs and rabbits showed that the heart could be stopped during surgery for around 15 minutes and then successfully started again without causing any ill-effects. Complicated heart surgeries required the heart to be stopped for far longer than 15 minutes, but leaving the heart without blood for such lengthy periods led to serious tissue damage.Extensive testing in rats offered the answer.
In the 1980s, researchers at St Thomas’s Hospital found that by cooling the heart to below 28°C and treating it with the right cocktail of chemicals, the heart could be stopped for many hours while intricate surgeries were performed, and then restarted with minimal damage. A similar cocktail of chemicals is now used to keep hearts healthy while they are transported for transplantation.
Today, the heart lung-machine, which was invented and perfected through a series of animal experiments, is commonly used to do the job of the heart and lungs for many hours, enabling complex and time-consuming cardiac surgeries to take place. The machine is also essential for keeping patients alive during heart transplants, and has formed the basis for techniques that support premature babies and those with respiratory or cardiac problems for more extended periods
History of the heart-lung machine