The fact that many possible drug compounds fail to make it to market has long been twisted by animal rights activists to suggest that this is in some way the fault of animal studies. The claims commonly take the following forms:
“90% drugs tested on animals fail” – Cruelty Free International
“92% of drugs fail in clinical trials, having successfully passed through animal studies” – Safer Medicines Trust
“In fact according to the FDA’s research, nine out of ten drugs deemed successful in animal tests fail in human clinical trials” – Humane Society International
Of course, this high attrition rate has little to do with animal studies being ineffective as Royal Society Fellow Professor Robin Lovell-Badge explains here. Indeed, animal studies within the narrow context of drug testing (which is a relatively small area of animal research), are not expected to be completely predictive, as indeed human trials are not, since sometimes it is not until a drug is made available to the general public that rare side-effects are encountered.
However, a high attrition rate does beg the question as to why and where compounds ‘fail’ in their journey through preclinical (animal, computer and other lab-based testing), and three stages of human clinical trials.
Some insight into this question lies across a number of papers which often have a different focus but nonetheless provide insight. In one such paper from 2015, four pharmaceutical companies, AstraZeneca, Eli Lilly, GlaxoSmithKline and Pfizer, pooled their data for a paper published in Nature Reviews | Drug Discovery which helped to quantify the when and whys of the situation.
The focus of the paper was on the physicochemical properties of small-molecule compounds and showed for the first time that control of physicochemical properties during compound optimization is beneficial in identifying compounds of candidate drug quality whilst indicating, also for the first time, a link between the physicochemical properties of compounds and clinical failure due to safety issues.
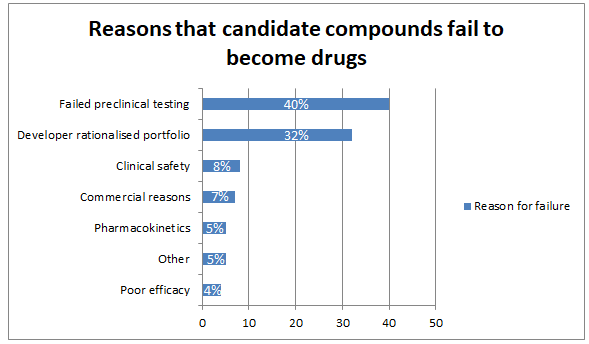
Along the way, however, it was able to attribute causes of failure to other factors. Between 2006 and 2010, for instance, the greatest reasons for failure were negative results following non-clinical toxicology i.e. computer modelling, cell cultures, animal tests and all other non-human methods, which put an end to 40% of compounds. In other words, these tests were successful in screening out compounds that were potentially harmful to humans. However the number two reason was the rationalisation of a company’s portfolio away from a particular area of drug development which caused a further 32% to be withdrawn. Following this there is a big drop to the 8% attributable to clinical safety – compounds which were found to be harmful or not tolerable in human volunteers - which manifested equally in phases 1 and 2 of clinical trials.
Commercial reasons, such as a rival getting a product to market before the candidate compound could be approved, accounted for a further 7%. Poor efficacy was responsible for just 4%, pharmacokinetics a further 5% and other causes combined – formulation, patent, scientific and regulatory issues - came to another 5% (all figures rounded up to the nearest whole number).
The authors also speculate that the pharmaceutical industry’s investment in screening for genotoxicity, compounds which inhibit the hERG channel (acting on a gene that’s important for heart function) and detecting drugs with lots of off-target effects was increasingly halting compounds before they got anywhere near either animal or human tests.
The broader takeaways from the paper are really that this type of collaboration between pharma companies is the way to go for creating new insights into the causes of drug attrition, since an individual company is unlikely to have enough data to form robust conclusions on its own. Progress is likely to be incremental because the causes are diverse and complex, often owing more to the commercial than the clinical. What is clear once again, however, is that the tired old meme that most drugs fail in humans after working in animals is the wrong conclusion to draw in the light of the available evidence.
Last edited: 20 May 2022 16:00


