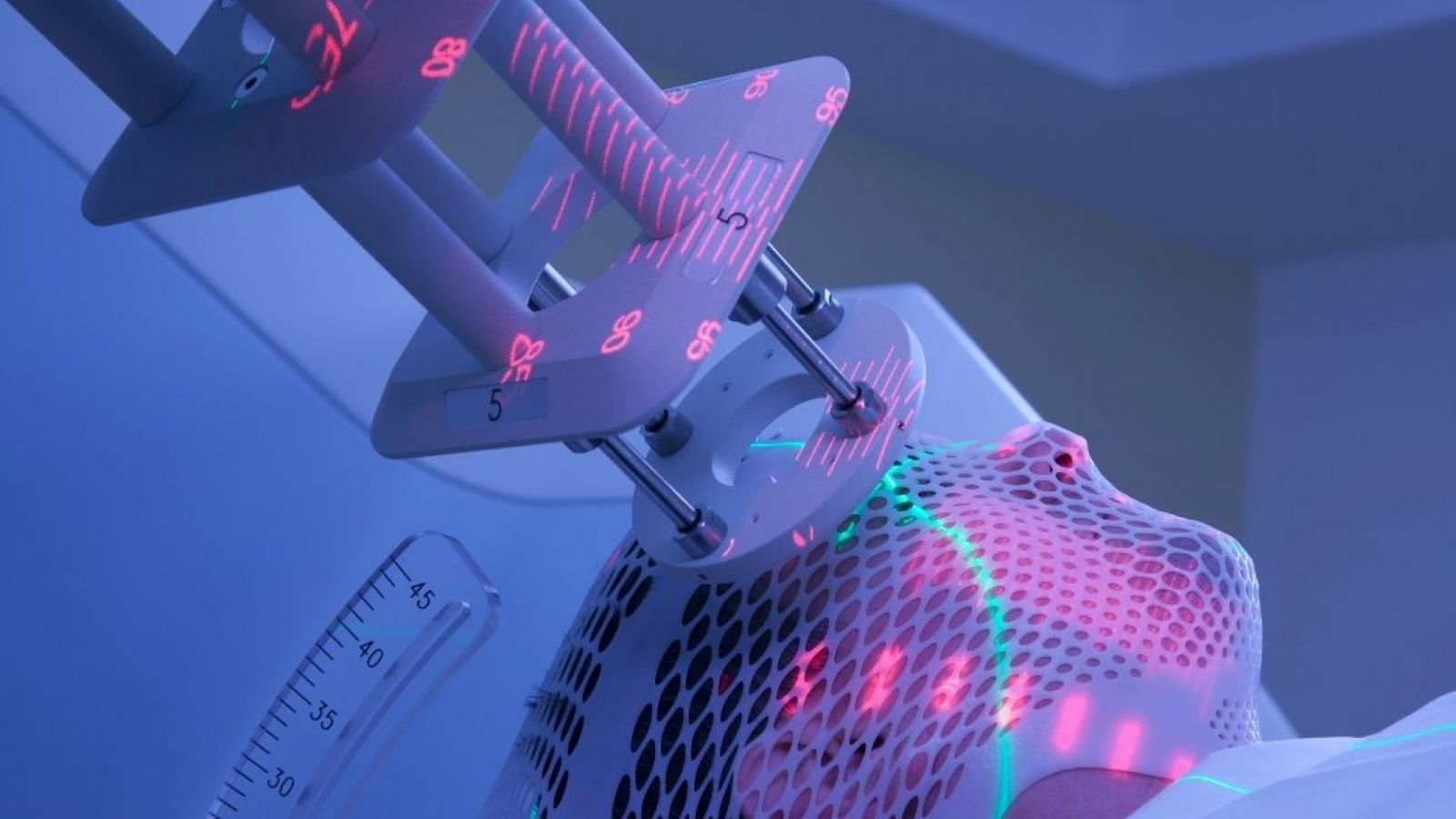
Radiotherapy is a powerful tool in treating cancer, but it is a blunt instrument. In some cases the radiation can be as lethal as the cancer and so treatment regimes must always play a balancing act. We know that stronger doses of radiation work better to kill the cancer, but they also do more damage to the rest of body. This is why much effort goes into refining the technique and minimising collateral damage.
Research from the University of Michigan, published online this week at Nature, has yielded a technique of making the body more resilient against radiation. Jian-Guo Geng and colleagues have found two proteins, Slit2 and R-spondin 1, which target a receptor found only on the surface of intestinal stem cells. When these proteins bind to the receptor, they boost the power of stem cells to repair damage to the lining of the gut caused by radiation.
Although they lack the glamour of the heart or the brain, the intestines are a crucial point for keeping a patient alive. Damage to the lining can prevent the body from absorbing necessary nutrients from food. Perhaps even more importantly, the tissue of the intestine ensures that the gut bacteria stay where they are and don’t escape into the bloodstream.
The gut naturally contains a store of stem cells for repairing damage, but the power of the radiation means that they are overwhelmed. When either Slit2 or R-spondin 1 is added, the stem cells become more active. This effect is increased further when the two proteins are combined as they work better together.
The effects were first observed in cells extracted from mice, where the researchers could investigate the mechanism behind the activity. The same experiments were then done with mice to test larger-scale survival and the robustness of gut function. The mice that were injected with these proteins could withstand much stronger doses of radiation than control mice. When exposed to a lethal dose, all of the untreated mice died while 50% of those with Slit2 and R-spondin 1 survived. The scientists remain optimistic that they can get this percentage higher with further research.
While it might take over a decade before this can be used in humans, if at all, the prospect of more effective radiotherapy raises hopes. Radiotherapy is often used in late-stage metastatic cancers, where the cancer has spread to different parts of the body. At this stage, the cancer could be terminal and treatment can only hope to slow the growth. If patients can withstand stronger doses of treatment then more cancers than before could be eradicated.
Last edited: 3 August 2022 10:48